On April 9th, the Internet of Things Consortium (IoTC) gave a webinar titled “Connected Health and Wellness,” hosted by Greg Kahn, President and CEO of the IoTC. He said this telehealth webinar was the first of a series of bi-weekly webinars on the Internet of things. The next IoTC Now event will be on April 23 and will discuss the connected home.

Earlier, on April 2nd, the IoTC had added connected health and wellness as one of five core verticals to advance IoT growth and adoption. There were actually four additional speakers beyond the ones shown who presented at the webinar, but they didn’t really discuss telehealth or telemedicine.
 Key participants of the IoTC Collected Health and Wellness webinar. (Credit: IoTC)
Key participants of the IoTC Collected Health and Wellness webinar. (Credit: IoTC)
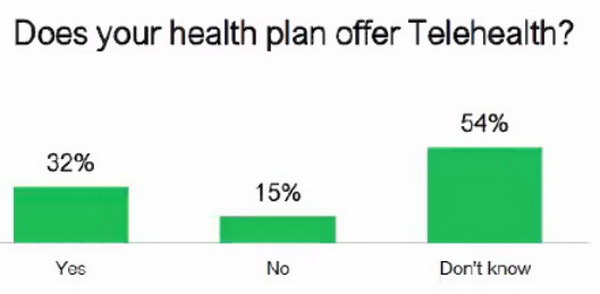 A majority of consumers don’t know if telehealth is available to them. (Credit: JD Power 2019 U. S. Telehealth Satisfaction Study)
A majority of consumers don’t know if telehealth is available to them. (Credit: JD Power 2019 U. S. Telehealth Satisfaction Study)
James Beem of JD Power discussed telehealth and the 2019 JD Power study of the field. One of the big barriers to telehealth is consumers simply don’t know about it. Typically, they don’t know if their medical provider provides telehealth services or their insurance company will pay for it.
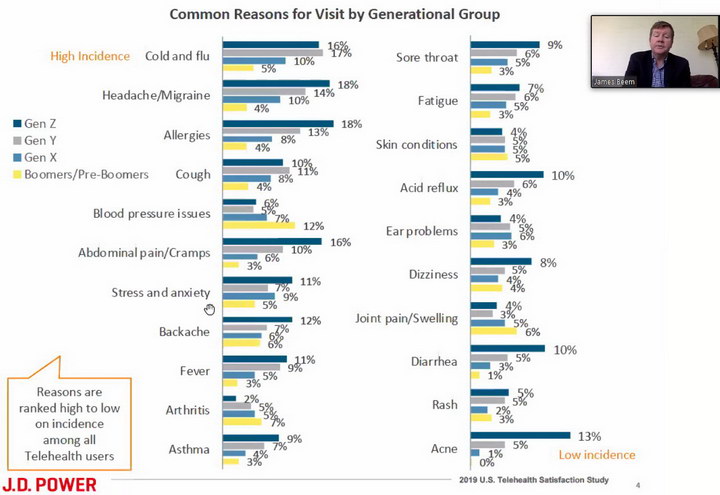 Telehealth Usage by medical problem and generation. (Credit: JD Power 2019 U. S. Telehealth Satisfaction Study)
Telehealth Usage by medical problem and generation. (Credit: JD Power 2019 U. S. Telehealth Satisfaction Study)
As part of it’s 2019 study, JD Power examined the usage of telehealth by medical problem and generation. Clearly Gen Y (now 26 – 40 years old) and Gen Z (now 5 – 25 years old) are the heaviest users of telemedicine. These people are digitally enabled and talking to a doctor or a nurse via a video link would be nothing new to them, since they are accustomed to talking to friends, family and business associates via links like Skype and Zoom. Boomers (now 56 – 76 years old) like me use telemedicine the least – I know I don’t use it.
The most common use of telehealth is for cold and flu, not surprising since there is little a doctor can do about it except say “drink plenty of fluids and go to bed.” If necessary, the doctor can prescribe medicines such as cough medicine or decongestants based on the video conference. These prescriptions are already transmitted directly to the pharmacy, not given on paper to the patient, and telehealth will not change that.
There is also a wide variation in the medical problems addressed by telehealth and these problems varied by age group. Essentially no boomer consulted a doctor via telehealth for acne but they consulted the doctor more often than other generations for blood pressure problems. No surprise with either of these findings.
 Amwell products serving the telehealth market. Left, software running on consumer displays; Center, K40 kiosk designed to be used in non-medical facilities; C760 cart for use in medical facilities. (Credit: Amwell)
Amwell products serving the telehealth market. Left, software running on consumer displays; Center, K40 kiosk designed to be used in non-medical facilities; C760 cart for use in medical facilities. (Credit: Amwell)
Telehealth comes in three different flavors and American Well (Amwell) provides hardware and software for all three types, as shown in the image. As would seem obvious, there is a display and camera at both ends of a telehealth link. The three flavors are:
- Patient-to-doctor or nurse when the patient is in some location other than a medical facility, most commonly at home. In this case, the patient most commonly would use the same display and camera he uses for other applications, his smartphone, tablet or laptop computer. The doctor or nurse in their office may also use a laptop computer.
- Patient-to-doctor or nurse when the patient is in a non-medical facility equipped with specialized telehealth hardware and software. One example of this is a remote telehealth facility at a work location or in a “Minute Clinic” in a drugstore. Another example is when a patient needs to consult with a doctor or nurse who is not on the premises. For example, in a psychiatric Emergency Department (ED), a patient can talk to a psychiatrist who may be off-site.
- Doctor or nurse consulting with a medical expert in a particular problem who is not available on-site.
In addition to the main hardware unit and software, Amwell supplies a number of connected accessories that provide information to the doctor or nurse from the remote location. These include several high-resolution, medical grade hand-held cameras such as a dermatoscope for examining skin and an otoscope for looking into ears; digital stethoscopes; a pulse oximeter; a blood pressure cuff; and a thermometer.
For some, telehealth and telemedicine may be a time and money saver. For others, especially people in remote areas, it may be a life saver. For example, John Dolbinski, Director of Medical Imaging Services of the Alaska Native Tribal Health Consortium (ANTHC) recently said,
“ANTHC’s mission is to meet the unique health needs of more than 175,000 Alaska Native and American Indian people living in our state. Our medical center is the state’s main referral site as an Adult and Pediatric Level II Trauma Center, and provider of primary and specialty care. Increasing our capabilities in telehealth, teleradiology, data exchange and connections beyond Alaska are critical to fulfilling our mission.”
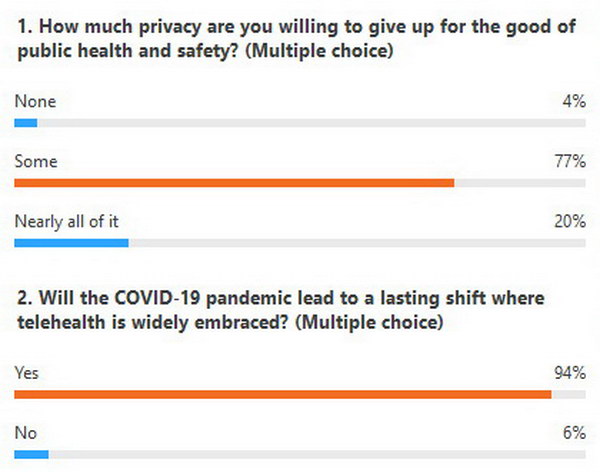 Survey of telehealth webinar participants. (Credit: IoTC)
Survey of telehealth webinar participants. (Credit: IoTC)
At the beginning of the webinar, Mr. Kahn asked participants to answer two simple questions related to telemedicine. The second, “Will the Covid-19 pandemic lead to a lasting shift where telehealth is widely embraced?” the participants overwhelmingly said yes. No surprise there! The first question, however, “How much privacy are you willing to give up for the good of public health and safety?” I find more problematic and was one of the few people (only person?) who answered ‘None’ for several reasons.
- Giving up privacy on the Internet is forever but the Covid-19 crisis will pass.
- Medicine has strong privacy rules and regulations and these medical privacy rules make sense.
- For “free” services like Google, the company gets paid with information. Medicine is not and will not become a free service, even with telemedicine. Since medical providers are already well paid, there is no need to provide them with free information they can sell, too. If you are from Gen Z and ask your doctor about your acne, do you want to get bombarded with acne advertisements next time you do a Google search?
Other industries, such as banking, stock trading and prescription drugs, have managed to maintain privacy in a digital era, so put me down in favor of maintaining medical privacy rules, even with Covid-19 and telemedicine. – Matthew Brennesholtz

